- Tomography/3D imaging
- Instrumentation
- Acquisition mechanics
- Image reconstruction, units
- Image quality
- Radiation dose in CT
- Implications, typical doses
- Clinical applications
- Specialized techniques
- DECT, 4D CT, CBCT
- Specialized techniques
Tomography/3D imaging
“Tomos” means cut, cutting, slice, section, while tomography refers to a device/method to create an image where the object is visualized by “cutting” into section. A tomogram is the image that is created. Computed Tomography (CT) almost always refers to x-ray computed tomography, although other types (PET/SPECT) also exist. Instead of a single x-ray from a single direction, multiple x-rays from many different angles around the patient are taken. Images are typically produced through reconstruction from the multiple projections. Reconstructed images don’t have overlapping structures like planar x-rays, which has the main advantage of improving contrast.
To quantitatively illustrate the improved contract, below is shown a grid representing an extremely simple CT slice, with just 9 voxels. The center voxel has a value of 20, and the surrounding voxels have a value of 10. If we were to instead take a single projection from this slice, we would get a column of values 30, 40, 30 (summation of rows). The contrast of the slice is (20-10)/10 = 1.0. The contrast of the projection is (40-30)/30 = 0.33.
| 10 | 10 | 10 |
| 10 | 20 | 10 |
| 10 | 10 | 10 |
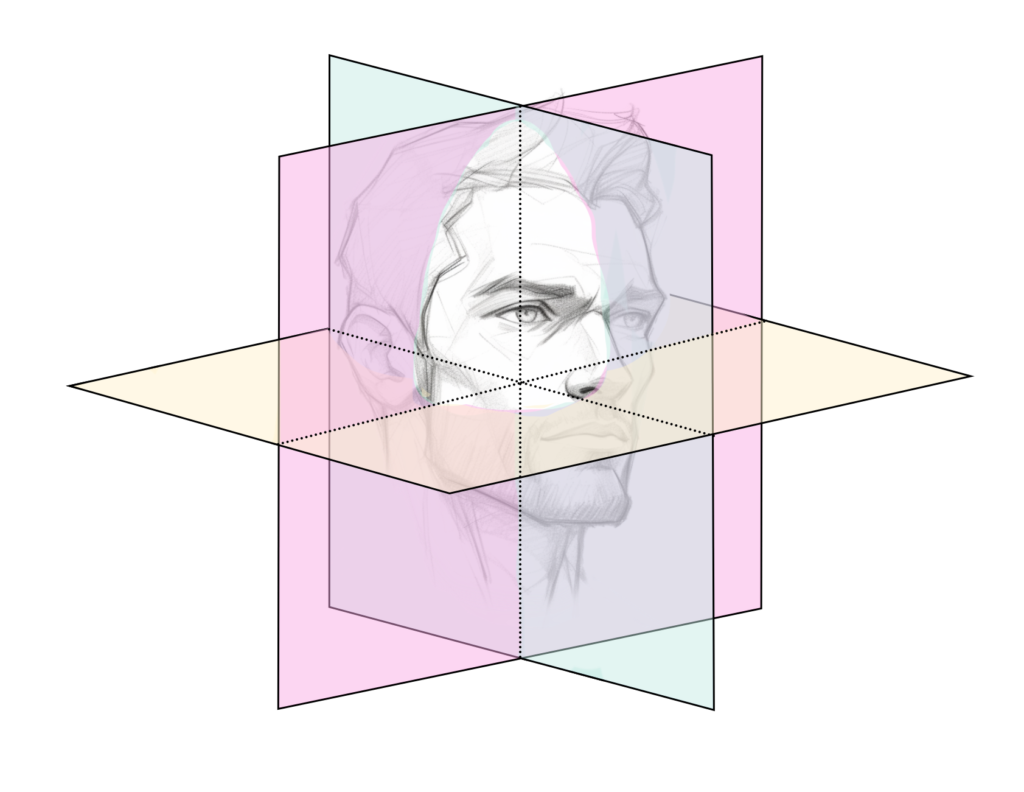
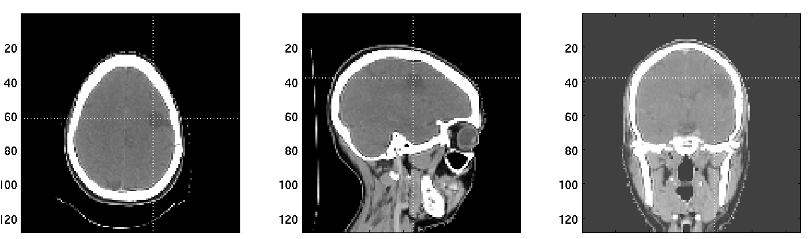
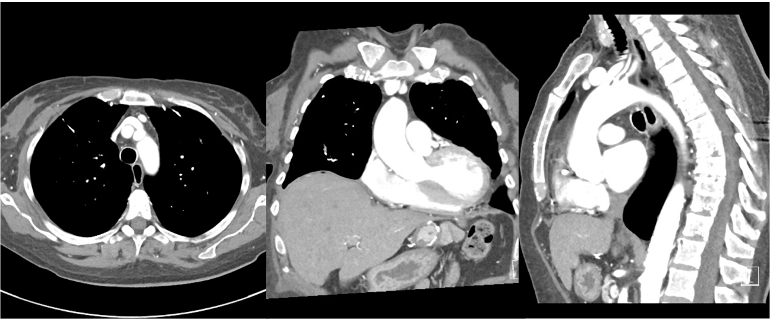
Imaging planes
Because we now have 3D images, it is important to define imaging planes since we still view images in 2D slices.
The canonical orientations are axial/transverse, coronal, and sagittal.
Axial/transverse: cross-sections of the body, horizontal slices looking up from the feet. This is the most common view for CT images, although others are also used.
Coronal: view facing the subject.
Sagittal: view from the side of the subject
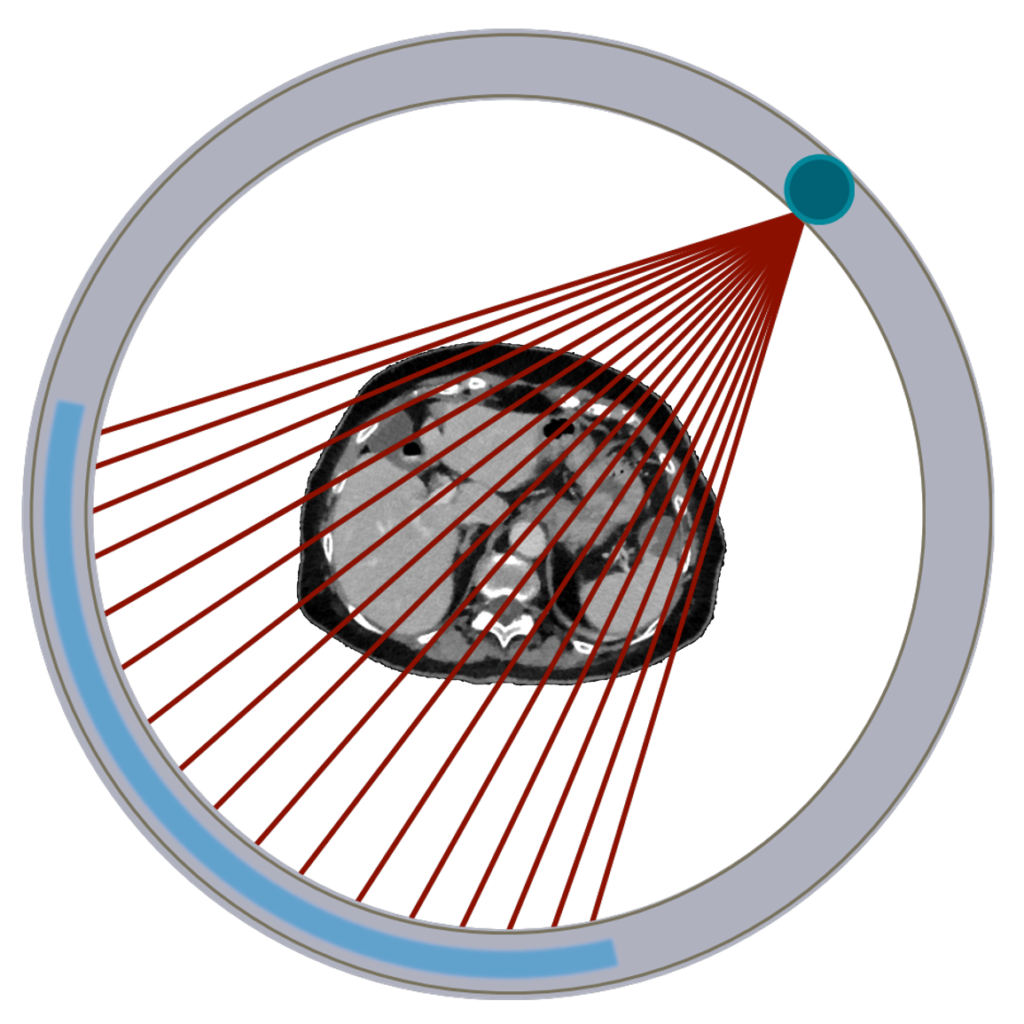
Instrumentation
In the past CT scans were called CAT scans for “computed axial tomography” since axial slices were acquired at multiple locations. Since moving away from strictly “axial” imaging, the “A” has been dropped. CT scans consist of a narrow fan-shaped beam of x-rays. Those x-rays are directed into a subject and some pass through to the opposite side and strike a detector, which can then form an image. The source and detector rotate around subject to acquire projections in ‘every’ direction. These projections are reconstructed into a 3D image.
The x-ray tube and detectors are aligned opposite each other so that the geometry is fixed as they rotate around the patient. This is important when reconstructing the 3D image from projections. The detector is curved to match the curve of the circular motion within the bore. The x-rays are collimated to desired thickness and fan-angle width, which is usually around 60 degrees. One rotation of the system will result in a single axial slice of the patient. The width of this slice depends on the width of the detectors and the collimation used. The patient is moved through the circular aperture (“bore”) while gantry spins 360° sending x-rays through subject to detectors. By moving the patient it is possible to get multiple slices that can then be stacked into a 3D image. Typical bore sizes are 65-80 cm, sometimes larger for radiation therapy applications. For CT systems used to plan radiation therapy, gantries can be tipped up to 30° to allow for non-axial imaging and achieve the desired setup.
X-ray tube
The x-ray tubes used in CT scanners operate with the same principles as those for planar imaging. They typically have large and small focal spots and a rotating anode to dissipate heat. The heat loading is extra important in CT imaging because so many images are taken in a row – the tube may need to run continuously for minutes in some applications. The main settings for the x-ray tube are kVp and mAs.
Collimation and compensation
Pre-patient collimation limits the field-of-view using lead or tungsten blocks. Like with planar x-rays, collimation is useful for reducing dose and improving image quality by limiting scatter radiation. Collimators limit the beam to total size of detector array. For systems with a single detector row, collimation determines the slice thickness. For systems with multiple rows/slices, the thickness is determined by the detector and reconstruction options.
Post-patient collimation further reduces scatter radiation by placing septa between detector elements. These septa stop large angle scattering and help improve contrast. This is similar to the anti-scatter grid used in planar x-ray. The septa can be 1-D (rows) or 2-D (grid).
Compensating filters are used between the tube and the patient to account for the typical patient shape. A bow-tie filter is used to reduce beam intensity on periphery of beam, where body is thinner and more photons are able to pass through. The edges of the filter are thicker than the center to stop more photons at the edges. Filters are typically made of metal (e.g. aluminum, copper) and plastic (lightweight and easy to shape).
These filters also partly correct for beam hardening, where the energy spectrum of x-rays changes with thickness. Lower energies preferentially absorbed as a multi-energy beam passes through a material, such that a higher proportion of higher energy photons pass through. Additionally, by filtering some of the unnecessary x-rays, these filters also reduce dose to the patient.
Detectors
Geometry
CT scanners were originally designed with one row of detectors, but most modern scanners have multiple detector rows (MDCT) – anywhere from 16 to 320! With multiple rows it is possible to acquire several slices during each gantry rotation and it reduces demands on x-ray tube.
Materials
CT detectors are solid-state scintillators and have high x-ray detection efficiency. They use a crystal that emits light when struck by the x-rays from the x-ray tube. Scintillation crystals (Gd2S2O, CsI, and other materials as well) are sintered to increase physical density and light output.
Sintering is when scintillation powder is converted into high-density ceramic using heat. The high density helps with detection efficiency. These crystals are scored to create individual detector elements. A photodiode is connected to the scintillator to convert light photons to electronic voltage, which can then be processed into image intensities. The size of the detector elements is one aspect that contributes to the resolution of the system.
These detector arrays are curved to match the x-ray beam and the rotation within the bore and typically cover around a 60° angle. They are divided into modules to allow for easier repair if a detector element malfunctions. Each module has processing electronics to amplify and refine the signal, and an ADC to store data as digital bit. Final processing is done on the computer to form images.
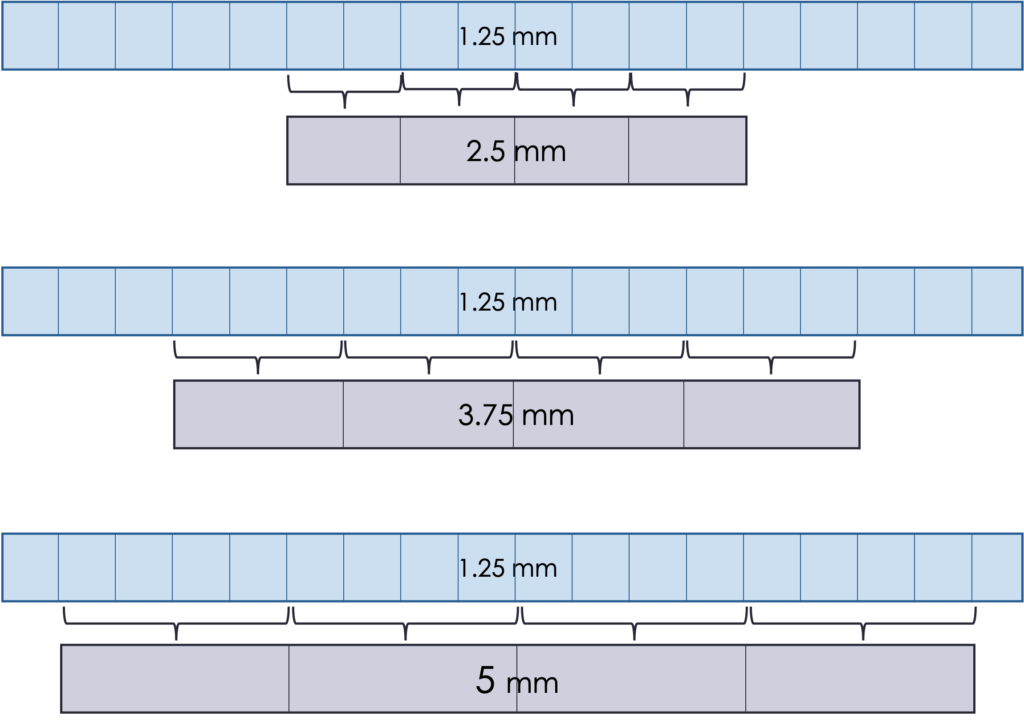
The detector size determines the minimum slice thickness, which is typically 0.5 to 1.25 mm. It is possible to group elements to create thicker slices. This is typically done at the reconstruction stage.
What is the consequence of thicker slices? Think about SNR and spatial resolution
Thicker slices mean better SNR because there is more data in every slice (higher N). However, the spatial resolution is worse because more information is being averaged and fine details become blurred.
Another consequence is that thicker slices can mean a reduced radiation dose. More photons are contributing to each slice, so fewer photons are needed overall to maintain the same SNR. It can also be quicker to acquire, which is important if the patient may have trouble staying still (pediatric, breath hold, trauma, etc.).
It is also quicker to read the slices, or create contours for radiation therapy, if there are fewer slices covering the area of interest. The choice of slice thickness depends on the clinical situation.
An example of the effect of different slice thickness in the abdomen is shown below. The 5 mm slices are less noisy but have worse resolution than 1 mm slice thicknesses. There is usually a “sweet spot” that balances SNR and resolution, but it depends on the clinical task and the anatomy imaged.

Acquisition mechanics
An important aspect of CT scanning is the scanner rotation and bed motion. Because CT is a 3D imaging modality, multiple slices must be acquired. Detector arrays as wide as a patient are prohibitively expensive, so instead the patient bed changes position so that the full axial extent desired may be imaged with a detector array that may be only 20 – 40 mm wide.
To acquire the multiple projections needed to reconstruct a 3D image, the tube and detector must rotate around the gantry. Since a high voltage is needed constantly to produce x-rays and collect signal from the detectors, the system uses a slip ring assembly, where brushes maintain contact with the rings during the rotation. Most CT scanners can do up to 5 rotations per second, which result in high angular velocities and large g-forces. As such, the system needs to be carefully engineered and balanced to maintain these speeds safely. The x-ray tube must also be aligned with the axis of the scanner so that the cathode-anode run parallel to the z-axis. This configuration also allows for the wide (~ 60°) angle of the fan beam. A CT scanner can take 1000 – 3000 projections in a single 0.5 second rotation.
Axial
Originally CT scanners used an axial motion to collect multiple slices (hence the original name computed axial tomography, “CAT”, scan). In this setup, the gantry rotated around the patient, the bed moves to the next position, gantry rotates again, and so on until the full axial extend desired has been imaged (e.g. 30 cm to cover the lungs). This processes is somewhat slow and the total time depends on the beam width and length to be scanned.

Helical/Spiral
More commonly, modern CT scanners use a helical motion to acquire images. In this setup, the bed moves continuously while the tube-detector system rotate. This process results in faster imaging and greater dose control. The helical pitch determines the effective slice thickness and dose. Pitch is the distance the bed moves during one beam rotation, divided by the beam collimation. For overlapping motion, pitch is less than 1. Contiguous motion has pitch equal one, and extended motion has pitch greater than 1. The dose is roughly proportional to 1/pitch, such that higher pitches result in lower dose (less overlap). The final image slices are still axial and are reconstructed by averaging CT projections taken 180 degrees apart.
Question: if collimation is 10 cm and bed moves 20 cm per rotation, what is the pitch?
pitch = bed motion / collimation = 20 cm / 10 cm = 2 (extended)
Couch/bed properties
For best image quality (and comfort) scanners use a curved couch because it matches geometry of CT detector arrays. However, Radiation Oncology uses flat couchtop to match linac treatment couch, since treatment planning CTs must be taken with the exact same setup as treatments will have. The result of this is slightly worse spatial resolution and contrast.
Beds are made of carbon fiber to minimize x-ray attenuation (which otherwise reduces number of photons reaching detector and affects SNR). The bed can move up and down to help center the patient, and it moves the patient in/out of gantry. Bed motion can be manual during setup, and is automated (very precisely) during scanning. Beds do not move side-to-side, they stay centered in gantry bore. The couch has a weight limit, usually 400 or 500 lbs. It is important not to exceed the weight limit as it can cause the couchtop to sag and positioning to be off, and puts a strain on the mechanical motion system.
Projection Radiographs
While laser lights in the scanner bore can give a good idea of the centering of the patient and the axial range to scan, 2D imaging is often done before the full 3D CT scan. One or two projection scans are taken to verify positioning and define axial extent of imaging. The x-ray tube is placed either at the top of the gantry for anterior-posterior view, or at the side for a lateral view. With the tube in a fixed position, the bed moves through the scanner for a predefined length and creates a projection image over the distance moved. These initial scans often have different names for different manufacturers and can be referred to as scout scans, topograms, projections, scanograms, or localizers. After these scans, a dialog comes up for the technologist to adjust the axial range to include the desired anatomy.
Image reconstruction
CT coordinates are typically as follows: Z from superior to inferior(head to feet), X from right to left (patient orientation), and Y from posterior to anterior (patient orientation). Images are typically displayed in transverse/axial, sagittal, and coronal views. Transverse are in the XY plane, coronal in the XZ plane and sagittal in the YZ plane. Transverse are cross sections of the body looking up from the feet, coronal are shown as if facing the patient, and sagittal are from the side of the patient. See imaging planes.
The many projection images are put into sinogram format as they are acquired. The sinograms are a map of the intensity (number of photons) seen by the detector at a given angle and distance from the center. The intensity varies with the amount of attenuation of the photon beam passing through each part of the patient. See the section on image reconstruction for some details. CT typically uses FBP although there is more use of iterative reconstruction in recent years, especially with the push for lower doses, which is better handled with iterative recons.
Reconstruction parameters include pixel sizes (typically 0.5 – 1 mm), slice thickness (typically 1.25 to 5 mm), field of view (FOV), filtering and smoothing. Using the same matrix size, the FOV can be made smaller to achieve smaller pixel sizes. This is especially useful in head and neck imaging, where patients are smaller and more detail is needed. Filtering can be used to improve details (but also increase noise), or add smoothing (fewer details but less noise). CT scanner consoles typically offer several preset filters depending on the anatomy, e.g., standard, soft tissue, lung, chest, bone, detail, edge. They vary in the amount of smoothing/sharpening applied to balance resolution and noise.